May/June Issue of vein specialist
VENOUS2024: Not Your Grandparent’s Compression
Table of Contents
Message from Editor
Steve Elias, MD
Under Pressure: Evaluating Changes in Unna’s Boot Interface Pressure
Ismene S. Germanakos, Connie Koutsos, Antonios Gasparis, MD, and Nicos Labropoulos, MD, PhD
Optimizing Care: Compression Stockings in Varicose Vein Management– Evidence from CONFETTI Study
Amjad Belramman, MBBS, MSc, PhD; Roshan Bootun, BSc, MBBS, PhD, FRCS; Tristan R A Lane, MBBS, BSc, FRCS, PhD; and Alun H Davies, MA, DM, FRCS
Pneumatic Compression Makes Everyday Joys Possible
Jennifer Heit, PT, DPT, CLT-LANA
A New Treatment Choice That Keeps Patients Living Life
Maggie Thompson and Charles Liu
The geko™ Device: Breakthrough Technology for Post-Operative Care and Management of Venous Disease
Kieron Day, MD
New Treatment Paradigm and Associated Economic Impact for Managing Chronic Venous Disease via Mechanical Thrombectomy
Nicolas Mouawad, MD and A. Baqai, MD
What Patients Are Saying About JOBST® Compression Innovations
Margie Hopkins BS, MHA
Bandage-Free Venous Leg Ulcer Treatment
Sundaram Ravikumar, MD, MBBS, FRCS(C)
Empowering Patients, Clinicians, and Suppliers: USMCA Supporting the Lymphedema Treatment Act
Carmen Anderson
ElastiMed’s Wearable Device Will Knock Your Socks Off
Omer Zelka
Featured Article: 5 Traits CEO and Astronauts (Yes, Astronauts) Share
Korn Ferry Institute
AVF Associates’ Corner
Lorraine Loretz, DPM, NP
AVF to Lead Update of VLU Guidelines
Ruth L. Bush, MD, JD
EDITOR-IN-CHIEF
Steve Elias, MD
EXECUTIVE EDITOR
John Forbes, MBA
MANAGING EDITOR
Allie Sherrill
COVER ARTIST
Christine Rataj
PUBLICATION DESIGNER
Anthony Eaves
Message from the Editor

Steve Elias, MD
Editor-In-Chief, Vein Specialist
Member, AVF Board of Directors
The End of Time
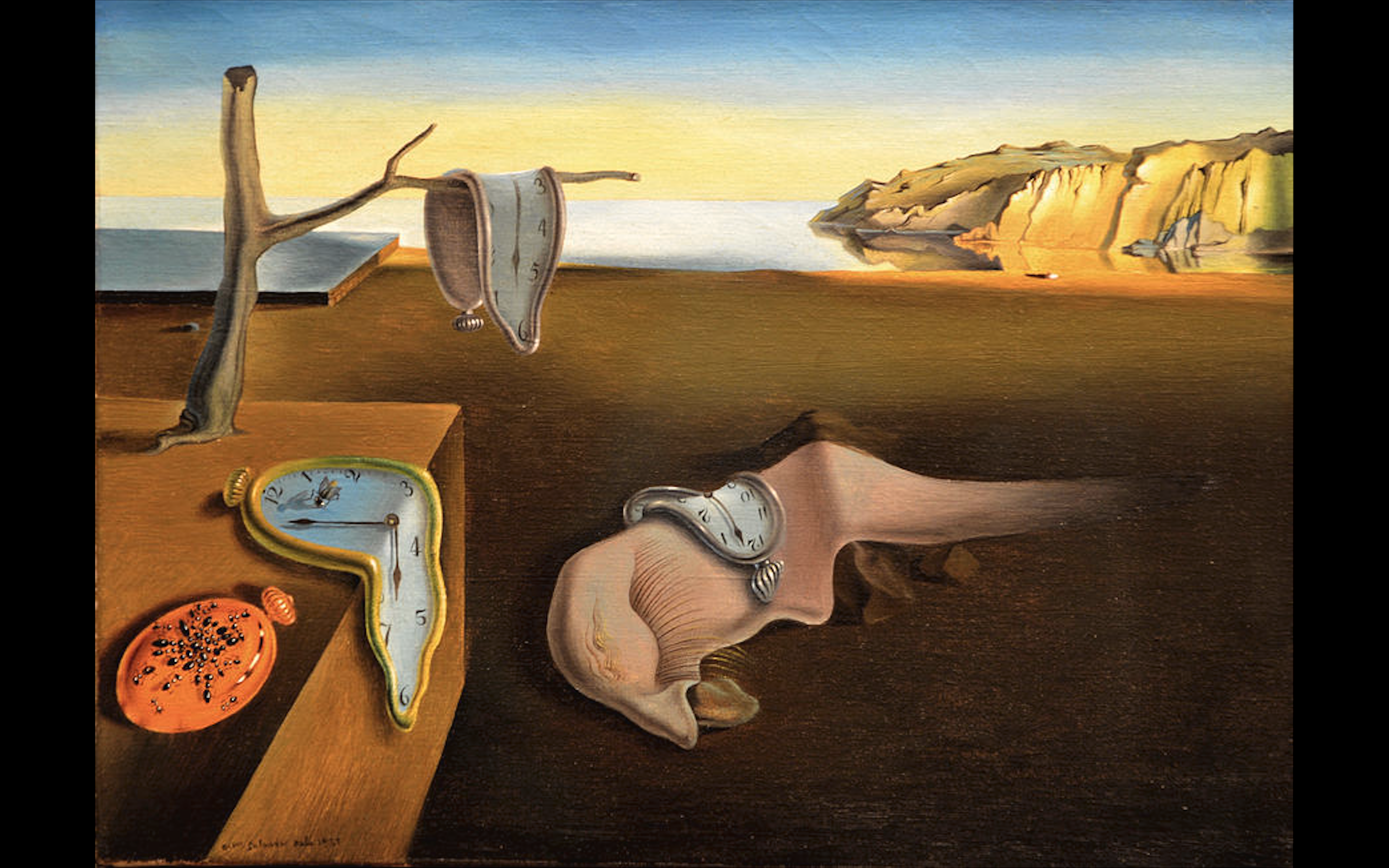
What happens when the promise of the new is no longer an option? Waking up becomes different. Do you exist in the “what is” and not the “what could be? ” Is the future replaced by the present, or worse, the past? Clint Eastwood (age 94), when asked how one should deal with getting older, answered, “Don’t let the old man in.” Especially if you are the old man. Delusional deception. But I like this advice. No matter what age, one should never let the old person in. It doesn’t encourage progress. Stagnation and/or regression ensues.
Signs outside NYC playgrounds say: “No adults allowed unless accompanied by a child.” They were initially posted so that the people who unfortunately get some perverted pleasure looking at children couldn’t gain access. But to me it evokes a mantra as to how to live one’s life. Live life as an adult with the outlook of a child: curious, non-judgmental, unjaded with an open mind. As vein specialists, our field is always evolving. We need to look at new ideas, techniques, technologies from the viewpoint of a child. Progress is never made by stodgy, traditional people. They are the hindrance. And they usually don’t recognize it. One’s outlook is more important than one’s age. To consider adapting anything new, one needs to feel comfortable with feeling uncomfortable. Embrace this concept and have confidence that everything will work out fine.
In this issue of Vein Specialist, we have articles about compression. Not the usual compression, but new ideas, devices, and technologies that bring compression into the modern era. From our Greek contingent we get an article that gives us a new understanding about evaluating the compression pressure attained by the tried-and-true Unna’s boot. And you thought, what could be new about this? “Optimizing Care: Compression Stockings in Varicose Vein Management– Evidence from CONFETTI Study.” Another way of looking at the use of compression in 2024 from our friends across the pond. Two articles discussing a new take on existing technologies highlight that in the end what we do is really about patient satisfaction: “Pneumatic Compression Makes Everyday Joys Possible” and “ What Patients Are Saying About JOBST® Compression Innovations.” Thinking like a child, we have articles about new unique devices. Approach these with an open, curious, non-judgmental mind: “A New Treatment Choice That Keeps Patients Living Life,” “The geko™ Device: Breakthrough Technology for Post-Operative Care and Management of Venous Disease,” “Bandage-Free Venous Leg Ulcer Treatment.” ElastiMed’s Wearable Device Will Knock Your Socks Off. These all give compression in unique ways. We have them here for you to know what is new. We’re just delivering the info; you make the decision.
The AVF Associates’ Corner is a new addition. We have a very important group of members who have a lot to add to good venous disease care, our associate members. Read about them. They were an integral contributor group to our last annual meeting. And it is about time we acknowledge their presence.

But time is a jet plane; it moves too fast. And time is a human construct that doesn’t last. It is arbitrary – seconds, minutes, hours. Who came up with this? The Babylonians and Egyptians way back when. A necessary evil to organize communal activities, public events, and cycles of planting and harvesting. Judeo-Christian teachings perceive time as linear. Incas and Mayans felt it was cyclical and continuous. In either case, time marches on. In 1765, scientist and physicist Joseph Priestelysuggested that time is one dimensional. All fundamental theories of physics are based on this. How boring. Anyone can think in one dimension. It takes a visionary to incorporate 2 or 3. Three-dimensional chess? The Glass Bead Game by Herman Hesse is a novel about boundless dimensions that are only restricted by the reader’s conceptual outlook. Einstein felt time was an illusion. Stephen Hawking described time as finite but boundless. The universe has no beginning or end but merely exists with a finite amount of matter and energy. Way beyond my mere mortal concept of time. As the group Chicago asked: “Does anybody really know what time it is; does anyone really care?” No matter what time it really is, it is 5’oclock somewhere as Jimmy Buffet reminded us.So have a drink and remember that it is always time to think young and the promise of the new is timeless. This issue of Vein Specialist brings you new ideas about the age-old concept of compression. Sit back, sip, and enjoy.
Under Pressure:
Evaluating Changes in Unna’s Boot Interface Pressure

Ismene S. Germanakos, BA
Research Assistant
Division of Vascular Surgery
Stony Brook Medicine

Connie Koutsos, BS
Research Assistant
Division of Vascular Surgery
Stony Brook Medicine

Antonios Gasparis, MD
Professor of Surgery, Zucker School of Medicine at Hofstra/Northwell
System Chief, Venous Disease Program
Division of Vascular and Endovascular Surgery
Northwell Health System

Nicos Labropoulos, MD, PhD
Professor of Surgery and Radiology
Department of Surgery
Division of Vascular Surgery
Stony Brook Medicine
Venous leg ulcers (VLUs), which affect up to 3 in 1000 people, often present as red, irritated plaques that develop into open wounds (Figure 1). VLUs may cause pain, itching, and swelling of the leg, as well as shame, embarrassment, depression, and loneliness. The Unna’s boot, a compressive multi-layer dressing, is considered the gold standard treatment for VLUs. Its zinc oxide-impregnated layer eases skin irritation, while its compression promotes venous return and reduces edema. While Unna’s boots may provide high interface pressure upon application, minimal data are available to evaluate what happens to the interface pressure after 7 days, the typical length of use. Therefore, our study aimed to evaluate the changes in supine and standing interface pressures after 1 week of Unna’s boot wear in VLU patients.
In this study, venous disease patients with active VLUs treated with Unna’s boots were selected from the same outpatient clinic. Demographic data were collected, and the interface pressure of the Unna’s boot was measured using the PicoPress device in both the supine and standing positions directly after applying the Unna’s boot and again after seven days at the follow-up appointment. A measuring probe was placed under the boot (Figure 2) in the leg’s most bulging area (B1 position). Patients with VLUs and recent venous intervention were excluded from the study.

Figure 1. Active Venous Leg Ulcer (VLU)

Figure 2. Measuring probe at the B1 position of the leg.
Ten limbs were enrolled in 9 patients with active VLUs (8 L; 2 R). The mean age, BMI, and ulcer size were 69 years, 32, and 5.2 cm2. Duplex findings showed venous disease in all patient legs (6 with superficial venous disease, 2 with combined superficial and deep disease, and 2 with deep venous disease). Our findings showed a significant reduction in interface pressure in the supine and standing positions at 7 days compared to baseline (Table 1). The mean Static Stiffness Index (SSI) at the time of application was 10.5 mmHg (inelastic range); after 7 days, it was reduced to 6.2 mmHg (elastic range).
Multi-layered compression bandages have been shown to have improved VLU healing rates compared to single layered bandages, presumably due to the higher interface pressure and improvement in venous hemodynamics. Our study shows a significant reduction in interface pressure after 7 days. Larger studies with daily pressure measurements are required to identify at what point after application a significant reduction occurs, which may change treatment protocols with earlier change of compression dressing. Technology that allows monitoring of interface pressure can indicate if bandages should be changed earlier in order to maintain inelastic compression, while improvement of compression devices that maintain high interface pressure over time may also improve clinical outcomes.
| Baseline Interface Pressure (mmHg) | 7 days Interface Pressure (mmHg) | ||
| Supine | Standing | Supine | Standing |
| 29 | 37.6 | 17 | 22 |
Table 1. Mean Supine and Standing Interface Pressures at Baseline and at 7 days.
Optimizing Care:
Compression Stockings in Varicose Vein Management – Evidence from CONFETTI study

Amjad Belramman MBBS MSc PhD
Honorary Clinical Research Fellow in Vascular Surgery
Imperial College London, United Kingdom
Omar Al-Mukhtar University, Derna, Libya

Roshan Bootun BSc MBBS PhD FRCS
Honorary Clinical Research Fellow in Vascular Surgery, Imperial College London, United Kingdom
Vascular Fellow, St George Hospital, Sydney, Australia

Tristan R A Lane is MBBS BSc FRCS PhD
Consultant Vascular Surgeon at Cambridge University Hospitals NHS Foundation Trust
Honorary Clinical Senior Lecturer, Imperial College London, United Kingdom

Alun H Davies MA DM FRCS
Professor of Vascular Surgery, Imperial College London and Honorary Consultant Vascular Surgeon, Imperial College Healthcare NHS Trust, London, United Kingdom
Corresponding Author:
Prof Alun H. Davies, Section of Vascular Surgery, Department of Surgery and Cancer, Imperial College London, 4N12A, Charing Cross Hospital, Fulham Palace Road, London W6 8RF, United Kingdom. Email: [email protected]
In our continued effort to enhance postoperative care for varicose veins, we have been investigating the effectiveness of compression stocking. While wearing compression stockings is recommended to help reduce swelling and pain, there has been a debate about their benefit post-treatment using ultrasound-guided foam sclerotherapy (UGFS). We are thrilled to share with you the findings from the CONFETTI study1 which sheds new light on this topic in question.
The CONFETTI study, a randomised controlled trial, was designed to answer the following question: Do compression stockings really make a difference after UGFS of non-truncal veins? We had 139 participants who were randomly chosen to either wear compression stockings for 7 days post-procedure or not. Our focus was to assess post-procedure pain after the procedure. Additionally, we evaluated at how compression affected the clinical severity, quality of life, occlusion rates, and complications.
The results show that participants who wore compression stockings reported significantly less pain than those who did not wear compression stockings. In addition, we observed improvements in clinical severity and quality of life in both groups, indicating the overall effectiveness of the vein treatment. This study did not identify any significant differences in other secondary outcomes such as return to normal activities and work between the two groups, though there was better generic quality of life in the non-compression group at 6 months.
While the CONFETTI study provides useful findings, we must acknowledge its limitations. The small sample size limits generalisability. Additionally, dropouts and compliance issues may have influenced the outcomes. We relied on subjective pain assessment, and the follow-up duration was short. However, it does answer the key questions about the early post-intervention phase.
The CONFETTI study has provided us with evidence about the benefits of compression stockings in post-foam sclerotherapy for varicose veins. They do help to reduce post-procedure pain, and UGFS overall as a vein treatment is effective at enhancing clinical severity and quality of life.
We must recognize that the field of varicose vein treatment is continually evolving. New approaches and technologies are being developed to enhance patient outcomes. As we learn more from studies like CONFETTI, it opens the door for more studies such as investigating whether the consistent usage of compression therapy after foam sclerotherapy affects the long-term re-intervention rates for patients with varicose veins? This question, among others, continue to inspire ongoing research and dedication to improving varicose vein treatment.
Corresponding Author: Prof Alun H. Davies, Section of Vascular Surgery, Department of Surgery and Cancer, Imperial College London, 4N12A, Charing Cross Hospital, Fulham Palace Road, London W6 8RF, United Kingdom. Email: [email protected]
Reference:
- Belramman A, Bootun R, Lane TRA, Davies AH. COmpressioN following endovenous TreatmenT of Incompetent varicose veins by sclerotherapy (CONFETTI). J Vasc Surg Venous Lymphat Disord. 2024;12(2):101729. doi:10.1016/j.jvsv.2023.101729