July/August Issue of vein specialist
Mistakes Made, Lessons Learned
Page 1 / 2
Table of Contents
Message from the Editor
Steve Elias, MD
Mistakes Made, Lessons Learned
When Not to Stent
Cees Wittens, MD
Ignoring the Obvious
Jose I. Almeida, MD, FACS
The Fishmonger’s Ice and the First CEA in Borås, Sweden
Bo Eklof, MD, PhD
Research Corner
V. Q & A: SVS/AVF/AVLS Guidelines on Varicose Veins Part I
Andrea Obi, MD, Peter Gloviczki, MD, PhD and Peter Lawrence, MD
Membership
Introducing the AVF Task Force on Inequities in Venous Care
Glenn Jacobowitz, MD, Misaki Kiguchi, MD and Ruth Bush, MD, JD, MPH
Join us at VENOUS2024
Arjun Jayaraj, MD
AVF Member named 2023 JVSVL Reviewer of the Year
Allie Woodward
Welcome New Members
May/June
Copyright © 2023 by The American Venous Forum. All rights reserved.
EDITOR-IN-CHIEF
Steve Elias, MD
EXECUTIVE EDITOR
John Forbes, MBA
MANAGING EDITOR
Allie Woodward
PUBLICATION DESIGNER
Gabi Graf
THE AVF CONFLUENCE: VENOUS JOURNAL CLUB SERIES
Facilitated by Dr. Mitchell Cox, Dr. Patrick Muck, Dr Michael Sadek, Dr. Gloria Salazar
Date: September 12, 2023
Time: 8:00-9:00pm ET
Sponsored by an educational grant from Cook Medical
Message from the Editor

Steve Elias, MD
Editor-in-Chief, Vein Specialist
XS and XXL and Beyond
Red wine spilled. On the shirt of my 5’ 11,” 185 lb, well-conditioned, lacrosse-player son. In Paris at Bouillon Chartier. Not many bouillons left in Paris. They were the workingman’s diner; their go-to place when they were hungry and needed an “honest meal.” Bouillon Chartier has many menu offerings: celery remoulade, leek vinaigrette, pork trotter, Felicie grilled, bouef Bourguignon, etc. Sound familiar? Yes, if you were a working-class Frenchman in the early 20th century. At that time, most working-class Frenchmen were not 5’11” and 185 lbs. They were 5’5” and 140 lbs in the 1920’s.
My son needed a new cheap shirt after spilling the wine. Hard to find in Paris in the 21st century. In Paris it is hard to find an XL shirt. The French, in general, have not attained this size. Large (L) is their upper limit of normal. Four stores later we found a shirt. Most native Parisians don’t need an American XL. For them, an American XL would qualify as an XXL or beyond. Or as they say, maxi-poitrine. An XL in France is equivalent to a US size 20 for women. There really is no such thing as a real S, M, L in the US now. I was always an S growing up. Now, to make us feel better in the US, an S is really an M. I now need to find an XS for clothes that fit. Semantics. The extremes of sizes. We deal with it all the time. My EPIC EMR has a default phrase, “patient is of normal stature and weight.” Conservatively, one-third of Americans don’t fit this description. I modify in EPIC. My brother-in-law, an internist, keeps telling me that I am the average size of a US soldier in WWII: 5’5,” 146lbs. In 2023, according to a Google search, the average weight of an American male is 198lbs. Height is 5’9” with a 40-inch waist. XL and beyond. The NIH estimates that 40% of us are obese. Don’t try to find clothes in Paris.
But you can find a lot of valuable information in Vein Specialist this month. We are not going back to WWII. This is 2023. We have challenged some of our brave contributors to write about mistakes made and lessons learned. Not always easy to bare one’s soul. We all learn from mistakes. The AVF/SVS/AVLS Guidelines are no mistake. They are thoughtful, cogent guidelines for the care of patients with superficial vein disease. Read the article that discusses how we got to these. Not easy. And some things aren’t equal. The AVF Taskforce will address inequities in venous care. Glenn Jacobowitz, Misaki Kiguchi, and Ruth Bush are leading the challenge.
I already alluded to the challenge of finding the right shirt as the red wine flowed and spilled on my son’s shirt at Bouillon Chartier. The drink also flowed for Richard Burton. He died in 1984. Brain bleed. Age 58. The Richard Burton Diaries was released in 2012. He was married to Elizabeth Taylor…twice. He loved her. I am sure Sir Richard spilled his share of wine, among other things. He had extra shirts available. Turnbull and Asser? Their James Bond collection? Average price for a shirt: $400. He could afford it. His dimensions are listed as: 5’10” and 165 lbs. He was no XL, XXL, or XS. Most likely a true 20th Century Medium.
Most of us don’t write diaries. Maybe we should. Vein Specialist can be thought of as the diary of the vein world. We try to reflect what is important in the vein world with each issue. And we give advice as to what is important. Our final words of advice: “America, it is time to stop growing”. BMI be damned. Let’s bring back S, M, L. Life would be simpler.
“When Not to Stent”

Cees Wittens, MD
Emeritus Professor of Venous Surgery
Rotterdam, the Netherlands
A 46-year-old man without any comorbidity suffered an iliofemoral DVT on the left side 5 years ago. He was suffering from severe venous claudication, so we suggested to recanalize the iliofemoral tract. Using magnetic resonance venography (MRV), we identified a diseased deep femoral vein (DFV), an occluded femoral vein (FV), and also occluded common femoral (CFV), external iliac (EIV), and common iliac veins (CIV).
We decided to create a good landing zone in the common femoral vein by performing an endophlebectomy and stenting the iliofemoral tract. Because of bad inflow from the DFV and FV, we also made an arteriovenous fistula with a 6-mm ringed thin-walled polytetrafluoroethylene (PTFE) prosthesis. During and after the procedure the patient received subcutaneous heparin and pneumatic compression of the calf.
Unfortunately, all occluded after 3 days, so we performed a thrombectomy and optimized the anticoagulation, which we thought might have been insufficient because the patient weighed more than 120 kg. However, 1 week later it occluded again, and we decided to keep it as it is and continue conservative treatment.
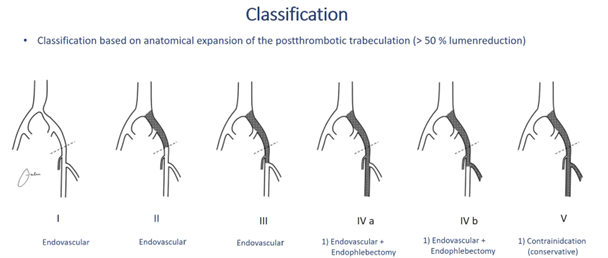
After this, we reviewed our last 100 cases and the lesson learned was that patients with such a poor inflow had a bad outcome. As published by H. Jalaie who reviewed more than 1000 cases out of multiple centers and developed a classification system, it was concluded that patients with such a bad inflow should not be treated due to bad outcomes. (1)
At the moment, we do not perform any recanalization in cases of a class V anymore.
Image courtesy of H. Jalaie
Reference:
- Jalaie H, Schleimer K, Barbati ME, Gombert A, Grommes J, de Wolf MA, de Graaf R, Wittens CH. Interventional treatment of postthrombotic syndrome. Gefasschirurgie. 2016;21(Suppl 2):37-44. doi: 10.1007/s00772-016-0156-4. Epub 2016 Jul 12. PMID: 27546987; PMCID: PMC4974289.
“Ignoring the Obvious”

Jose I. Almeida, MD, FACS
Founder, Miami Vein Center
Voluntary Professor of Surgery
Division of Vascular and Endovascular Surgery
University of Miami Miller School of Medicine
A 72-year-old woman presented to me with worsening lipodermatosclerosis over the left medial malleolus. She had a history of conventional saphenous vein stripping 30 years earlier at an outside facility. She had some small thigh and calf varicose veins bilaterally; however, her focus at the time of initial presentation was the indurated left ankle. Iliocaval duplex imaging showed a very tight left common iliac vein (CIV) stenosis and vein mapping of her superficial system showed bilateral saphenous remnants, which were refluxing.
In April of 2021 we placed an 18mm x 120mm Venovo stent in the left CIV in the office setting and she did very well. At her 1-month and 1-year follow-up visits she was very happy and ultrasound imaging showed her stent to be widely patent.
In December 2021, just prior to the Christmas holidays, she presented with bilateral lower extremity cellulitis. We prescribed Levaquin® 500 mg daily for 10 days and she improved clinically. In March 2022, she presented again with recurrent cellulitis and we gave her another course of Levaquin® antibiotic (Fig.1).
Figure 1. Cellulitis in March 2022.
In August 2022, she presented with her third episode of cellulitis. This time I picked up the ultrasound probe and had a look for myself. Ultrasound showed neovascularity at the groin with bilateral superficial axial reflux through large subcutaneous varicosities, coursing in and out of the saphenous canal in the thigh and extending to the ankle bilaterally. I must say I felt quite foolish for having prescribed antibiotics for 6 months for an obvious venous problem.
Two weeks thereafter, in August 2022, we treated her with ultrasound-guided, physician-compounded foam sclerotherapy and phlebectomy of the right leg. The following day, the same procedure was performed on the left leg. One month later, she came back for additional physician-compounded foam sclerotherapy of the remaining varicosities in the saphenous canal that did not close with the treatments one month earlier. I saw her again in December 2022, when her signs and symptoms showed marked improvement (Fig.2).
Figure 2. Following December 2022 sclerotherapy and phlebectomy.
The lesson learned here is that sometimes information from ultrasound technicians is not emphasized in the worksheet. I’ve always made it a habit for the past 25 years to have a small laptop ultrasound in my exam rooms that I use for a “quick look.” This patient presented with a focus on a left indurated ankle; and this diverted my attention away from her superficial system. Routine, superficial vein treatment resolved her problem for the time being. This patient will surely develop recurrent varicose veins in the future, so we are watching her closely every 6 months.
“The Fishmonger’s Ice and the First CEA in Borås, Sweden”

Bo Eklöf, MD, PhD
Lund University
Lund, Sweden
I did my 5-year surgical residency at the Central Hospital in Borås in southern Sweden starting in 1962. Alle Broomé, one of the Swedish pioneers in vascular surgery, was my tutor. In 1964 Alle spent one month at St Mary’s Hospital in London. Charles Rob had left for Rochester, NY, but Felix Eastcott was still active, so Alle could learn the CEA operation from him. At that time the procedure was performed under hypothermia.
Soon after Alle’s return to Borås a patient with recurrent TIAs and carotid stenosis presented. Together we planned the operation according to Eastcott’s protocol. The patient was placed on an inflatable bathtub which, after the patient was under anesthesia, was filled with cold water and ice cubes that we received from a fishmonger in town. The temperature fell accordingly to 32 degrees C, and it was time to stop the cooling and empty the bathtub. Alle and I were scrubbing, when suddenly we heard a scream from the OR and saw a flood of water pouring out. A wave had developed in the bathtub and 400 liters of water and the patient with all his tubes were on the floor. Nothing happened to the patient who carefully was replaced on the OR table. The temperature was now down to 29 degrees C, and we could safely proceed with the first CEA in Borås, without further events.
The fishmonger’s ice was probably more suitable for his fish, which were used to swimming in the waves. Four years later I started my Fellowship at Strong Memorial hospital in Rochester, NY, with Seymour Schwartz as my research mentor on compromised cephalic blood flow on cerebral function in baboons, and Charles Rob and Jim DeWeese as my clinical tutors.
Research Corner

Andrea Obi, MD, PhD
Chair, AVF Research Committee

Peter Gloviczki, MD, PhD
Mayo Clinic
Rochester, MN

Peter Lawrence, MD
UCLA Health
Los Angeles, CA
SVS/AVF/AVLS Guidelines on Varicose Veins Part I: Q&A
In March 2023, The 2022 Society for Vascular Surgery, American Venous Forum, and American Vein and Lymphatic Society clinical practice guidelines for the management of varicose veins of the lower extremities. Part I. Duplex Scanning and Treatment of Superficial Truncal Reflux were published in the Journal of Vascular Surgery: Venous and Lymphatic Disorders. (1) Senior authors Drs Peter Gloviczki and Peter Lawrence provided insight into the guideline development process for this issue of Vein Specialist. The guidelines abstract as it appears in the publication introduces their comments here.
Abstract: The Society for Vascular Surgery, American Venous Forum, and American Vein and Lymphatic Society collaborated to update the 2011 Society for Vascular Surgery/American Venous Forum clinical practice guidelines and provide new evidence-based recommendations on critical issues affecting the care of patients with varicose veins. Each recommendation is based on a recent, independent systematic review and meta-analysis of the diagnostic tests and treatments options for patients with lower extremity varicose veins. Part I of the guidelines includes evidence-based recommendations for the evaluation of patients with CEAP (Clinical Class, Etiology, Anatomy, Pathology) class 2 varicose vein using duplex ultrasound scanning and other diagnostic tests, open surgical treatment (ligation and stripping) vs endovenous ablation techniques, thermal vs nonthermal ablation of the superficial truncal veins, and management of incompetent perforating veins in CEAP class 2 disease. We have also made recommendations on the concomitant vs staged treatment of varicose tributaries using phlebectomy or liquid or foam sclerotherapy (with physician-compounded foam or commercially prepared polidocanol endovenous microfoam) for patients undergoing ablation of incompetent superficial truncal veins.
How did you decide on these major topic areas?
Gloviczki: The decision was not easy since there are so many important issues related to the management of chronic venous disease. The first decision we had to make was to decide on focusing these guidelines on C2 disease, on the management of patients with simple varicose veins. Reasons to do this were legion. The number of randomized controlled trials (RCTs) providing high level of evidence on long-term efficacy of different treatments for varicose veins has increased tremendously as we have at least 8 RCTs that have 5 -year follow-up and at least one that has 10-year follow-up. We ranked critical questions in order of importance and then we looked at the literature to see if these topics can be researched in a PICO format (patients, intervention, comparative test or treatment, outcome). It was essential to know we will have strong data of prospective comparative studies to support the guidelines. We also consulted the Mayo Clinic Evidence-Based Practice Research Program to ensure our decision was correct. Ultimately, we selected five major topics that were ranked highest for systematic review and meta-analyses and these data provided supporting evidence for Part I of the guidelines.
Lawrence: We addressed questions that had been raised in the literature and had not been adequately answered in the CMS MEDCAC session regarding appropriate treatment of venous disease. For example, the conclusion at MEDCAC was that there was inadequate evidence that duplex ultrasound was the diagnostic study of choice for varicose veins. So that was one of our first questions: what is the best diagnostic study for superficial venous disease? Other topics were ones that had been repeatedly discussed in the vascular literature, such as comparing outcomes between surgical stripping–which is still done in many parts of the world– and thermal ablation of truncal veins. In addition, questions about when perforator veins should be treated, and the timing of truncal ablation with tributary treatment- simultaneous or staged. Since there is a limit on the number of questions allowed with the PICO system of systematic reviews, there were other questions that could not be addressed in Part 1 and therefore were addressed in Part 2.
Why should venous specialists look to these guidelines compared to others for direction?
Gloviczki: There are many criteria that make clinical practice guidelines trustworthy and ours meet most of them. It is supported by an independent meta-analysis of the most recent high-quality data; less then 50 % of the writing group has any conflict of interest; we used the GRADE method to define the strength of the recommendations and the levels of the evidence; and the guidelines are based on the PICO format. In addition, our guidelines were reviewed by document review groups of 5 societies for approval and the document also underwent a public review.
Lawrence: These are multi-specialty and multi-society practice guidelines that are based on a systematic review of the literature. Single specialty practice guidelines are much less compelling and often do not have an impact on reimbursement by CMS, particularly if they disagree with other specialty guidelines. These guidelines were developed by the 3 vascular disease specialties who have venous disease training in their residency and who perform most of the superficial procedures for varicose veins.
In the ideal state, how will these guidelines be used?
Gloviczki: We hope these guidelines will be used by all venous specialists who treat patients with varicose veins. We also hope that third party payors will consider the recommendations and revise reimbursement based on the efficacy and cost effectiveness of the minimally invasive endovascular interventions, as reported in this document.
Lawrence: These guidelines should be used by venous specialists when they have questions about varicose vein treatment and in their discussions with patients. They should also be used by CMS and payors for reimbursement decisions. For example, the appropriate technique for preforming duplex ultrasound of truncal veins, partially in the standing or upright position, is critical in eliminating false positive and false negative studies. In a vascular lab that is not accredited or that does not use an appropriate technique for DU and that does not document the results so they can be reviewed, the treating physician may be performing unnecessary procedures. Hopefully, CMS and insurers will pick this up and only authorize procedures in patients who have had their DU study done in an accredited vascular lab, by trained personnel, and where the procedure images are recorded and done in the standing or sitting position.
What recommendations were controversial and why?
Gloviczki: The most controversial recommendation to me was the guideline on concomitant vs. staged treatment of varicose tributaries when the patient underwent saphenous ablation. We had multiple revisions and discussions to come up with the final guideline that supported a recent meta-analysis recommending concomitant treatment in most patients. The controversy was that we graded this strong recommendation with low level of evidence, because a sub analysis of 3 RCTs showed no difference in re-interventions between the study groups. In addition, 64% of the patients with planned staged intervention never had (or needed) a second procedure. In another RCT, the need for staged treatment of varicose tributaries was only 17% in those patients who underwent extended EVLA for axial, below-knee saphenous incompetence.
Lawrence: The timing of procedures, when there is both truncal (axial) reflux and tributary reflux received a lot of discussion, since some venous specialists stage procedures and some do them simultaneously. Ultimately, we agreed that simultaneous is optimal, based on the literature, but that there may be compelling reasons why patients prefer a staged procedure, such as time to return to work. So, this is an area where the decision regarding timing should be between the patient and physician.
Were you surprised by any of the data?
Gloviczki: I was surprised to find no evidence to support thigh perforator treatment in patients with competent proximal great saphenous vein (GSV) segment; large, incompetent thigh perforator; and incompetent distal saphenous vein. One would think this is an easy decision; these perforators need treatment right away. The literature, however suggested treatment for the incompetent GSV, without perforator interruption.
Lawrence: Even though the long-term outcomes of stripping and thermal ablation are almost identical, the early outcomes–particularly pain in the initial days after a procedure–were not well documented in many otherwise excellent studies. Therefore, ablation and stripping initially look similar in outcome, although all on the writing committee who had experience with both know that patient pain is significantly less with either thermal or non-thermal ablation. We were also surprised that there is little comparative data or prospective data on nonthermal ablation to allow the committee to compare nonthermal ablation to thermal ablation or stripping. Although nonthermal ablation of truncal veins is rapidly being incorporated in many practices, we need prospective comparative data– both short and long-term–of outcomes, including initial pain, superficial phlebitis, recanalization rates, and patient satisfaction, etc.
How will Part 2 of the guidelines fit in with the already published Part 1?
Gloviczki: Part 2 will fit to Part 1 perfectly. Part 2 discusses all remaining issues affecting the care of patients with varicose veins. These include the use of compression, the efficacy of medications and nutritional supplements, treatment of varicose tributaries, the management of superficial vein thrombosis, thrombotic complications of treatments, management of bleeding varicose veins, and the treatment of superficial vein aneurysms. Updates of previous society guidelines will address the management of venous ulcers, associated with varicose veins (C5-C6 disease), evaluation and treatment of deep vein obstructions and chronic pelvic venous disorders in separate documents.
Lawrence: Part 2 includes additional issues and questions that used a similar format to Part 1 but that were not part of the original PICO questions and that often had lower levels of evidence supporting them. Therefore, they required more discussion by the writing committees and debate before final conclusions were reached. This is part of developing practice guidelines; when lower levels of evidence exist, the writing committee should come to a consensus about best practices, even when the strength of evidence is not as strong and cannot be graded.
References:
- Gloviczki P, Lawrence PF, Wasan SM, Meissner MH, Almeida J, Brown KR, Bush RL, Di Iorio M, Fish J, Fukaya E, Gloviczki ML, Hingorani A, Jayaraj A, Kolluri R, Murad MH, Obi AT, Ozsvath KJ, Singh MJ, Vayuvegula S, Welch HJ. The 2022 Society for Vascular Surgery, American Venous Forum, and American Vein and Lymphatic Society clinical practice guidelines for the management of varicose veins of the lower extremities. Part I. Duplex Scanning and Treatment of Superficial Truncal Reflux: Endorsed by the Society for Vascular Medicine and the International Union of Phlebology. J Vasc Surg Venous Lymphat Disord. 2023 Mar;11(2):231-261.e6. doi: 10.1016/j.jvsv.2022.09.004. Epub 2022 Oct 12. PMID: 36326210.