Table of Contents
Message from the Editor
Steve Elias, MD
Message from the Guest Editor
Edgar Guzman, MD, FACS
New Year’s Dissolutions
Lyrics for a New Vascular World
Oscar Moreno, MD
DEI in the New Year
Kathleen Ozsvath, MD and Anil Hingorani, MD
Sexism in Research and Publishing: A trend on its way out
Andrea Obi, MD
2,800-Mile Step
Sebastian Cifuentes, MD
Rethinking thrombolytics and stand-alone anticoagulation in the age of advanced mechanical thrombectomy for the treatment of deep vein thrombosis
Venkat Tummala, MD
Thromboprophylaxis: An often-forgotten part of endovenous intervention
Benedict R.H. Turner, Matthew Machin, and Alun H. Davies
VENOUS2023
Kick Off Your Boots at the VENOUS2023 Gala
Roundtable Discussion with VENOUS2023 Program Chair and Speakers Venous Edge Video
Poster Session at VENOUS2023
Nasim Hedayati, MD, MS, MAS
DEI Session Invitation
Sheila Blumberg, MD, MS, RPVI
A Welcome Reception You Don’t Want to Miss!
Antonio Solano, MD
Medtronic Symposium Invitation
Stephanie Brucato and Daniel J. Denmark, PhD, MS
International
Introduction to the German Society of Phlebology
Erika Mendoza
Membership
AVF Health Policy Committee at Work for You AVF Health Policy Committee
Copyright © 2023 by The American Venous Forum. All rights reserved.
EDITOR-IN-CHIEF
Steve Elias, MD
EXECUTIVE EDITOR
John Forbes, MBA
MANAGING EDITOR
Allie Woodward
PUBLICATION DESIGNER
Christine Rataj
Message from the Editor

Steve Elias, MD
Editor-in-Chief, Vein Specialist
Dissolutions, Resolutions, Any Solutions?
The new year issue of Vein Specialist has traditionally had a guest editor. Last year and this year it is Edgar Guzman, a member of the newsletter committee. Vein Specialist looks at the new year. Edgar came up with the theme and the title. His letter follows. Before reading his, I leave you with some iconic opening lines of English literature to help you ponder the coming year. Food for thought. They speak for themselves:
- “In my younger and more vulnerable years my father gave me some advice that I’ve been turning over in my mind ever since.” The Great Gatsby, F. Scott Fitzgerald, 1925.
- “It is a truth universally acknowledged, that a single man in possession of a good fortune, must be in wont of a wife”. Pride And Prejudice, Jane Austen, 1813.
- “It was the best of times, it was the worst of times…” A Tale of Two Cities, Charles Dickens, 1859.
- “He was an old man who fished alone in a skiff in the Gulf Stream and he had gone 84 days without taking a fish.” The Old Man and The Sea,Ernest Hemingway, 1952.
And now read Edgar’s opening lines to this issue.
Message from the Guest Editor

Edgar Guzman, MD, FACS
Member, AVF Newsletter Committee
I don’t keep a diary, but if I did, I would hope my New Year’s entry would not be a list of (more) things to do and achieve in 2023. Rather, I would prefer to dissect where I am and how I got here and what I have learned in the process. I hope a clear course adjustment would emerge from it. Thinking of dissolution as a resolution.
So… what have I learned this past year? A key lesson was that when you say “yes” to something you are saying “no” to something else, whether you know it or not. That’s nearly self-evident, but nonetheless profound, because it acknowledges our finitude–only so many hours in a day and minutes of attention; only so many repetitions a body can endure. Failure to recognize this is a big part of why New Year’s resolutions fail.
Our culture abhors trade-offs; there is a definite negative connotation to the phrase. But does it follow that we are to endlessly accumulate more objects and undertake more activities?
Beyond being inevitable, these choices can be empowering. We need to start thinking of them as trade-ups. I had a few of those this past year. I got better at trading “me” time for family time; did less news reading and more book reading and spent more time with direct experiences rather than those mediated by a phone screen. I think I am the better for it.
Our authors in this issue share different experiences regarding changes much more significant than those above. You will see the common thread is their decision to say “no” to something that had ceased to be as important or simply recognized as flawed and saying “yes” to a better future.
Like our authors, let us be full of intention and hope when saying “no” and make way for better things to come. Sometimes it is better to dissolve to be able to resolve.
Happy New Year!
Lyrics for a New Vascular World
Oscar Y. Moreno Rocha, MD
Conrad Jobst Postdoctoral Research Fellow
Vascular Surgery, Michigan Medicine

In 1969, the Rolling Stones released the album Let it Bleed,, affecting millions of lives, including mine. Fifty-three years later a song from that album, “You Can’t Always Get What You Want” still affects my life.
I was born in Colombia and named after my father, who has been pursuing his dreams all his life. I was raised by the loveliest family I could ever wish for, and the most supportive. At a young age, I realized that I could do whatever I wanted because no one ever told me anything was impossible. I loved swimming, playing tennis, playing violin, painting, and photography, among my hobbies. I had a hard time choosing what pathway to follow for life. I wanted to do something that could change the world.

At first, it was hard to let go of the fine arts interests I had to become a doctor. Then, I fell in love with many fields of medicine. It is true what the lyrics of prophet Mick Jagger said, “You can’t always get what you want. But if you try sometimes, you just might find, you get what you need.” What a bloody album, you might think. But the truth is, none of us can do all the craziest ideas we come with or pursue all the pathways that open for us. We have to, at some point, be smart and let go of some. Literature describes soft and hard signs of bleeding, and the same could be said about success. Early signs that you might succeed in a field include becoming obsessed with it and loving it, which happened to me with surgery. Then I found I had an aptitude for surgical procedures. But the most crucial hard sign was fulfilling a more profound sense of identity. Surgical departments have personalities like the bands, and I have had the privilege of finding my perfect team. Quoting “With a Little Help from My Friends” by Lennon and McCartney, I discovered that I jump to begin new projects leaving behind some of them.

We know that in other regions of the world, such as in Colombia, conducting research is challenging. However, I was able to find a perfect storm under the mentorship of Andrea T. Obi, MD, at the University of Michigan as the 2023 Postdoctoral Research Fellow in vascular surgery and keep pursuing my dreams. I am here because I never thought anything was impossible; things just might take longer, and you will eventually make it. It is never easy to begin again in a new place, but there are indeed better things ahead than any we have left behind. As philosopher Stevie Nicks sang with Fleetwood Mac on the 1977 Rumours album, “You can go your own way.”
I want to thank the mentorship of Andrea T. Obi, MD, Thomas Wakefield, MD, Peter Henke, MD, and Sriganesh Sharma, MD, PhD, and all the members of the Obi Lab for helping me to pursue my wildest research and surgical dreams.
DEI in the New Year

Kathleen Ozsvath, MD
Membership Councilor, American Venous Forum
Member, AVF DEI Committee

Anil Hingaroni, MD
Member, AVF DEI Committee
Member, AVF Newsletter Committee
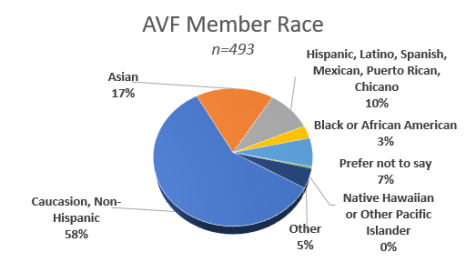
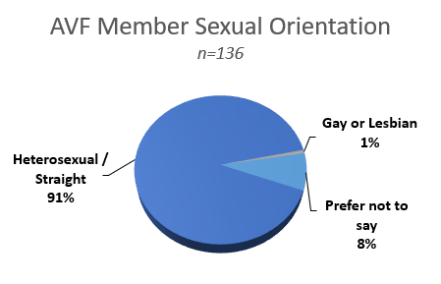
AVF membership is 23% female. Of the 118 AVF members who serve on one or more committees, 43% are female. Committee chairs are 36% female. In a survey sent to members, the following results were obtained regarding race and sexual orientation.
We must all work on creating environments that are inclusive, where diversity is celebrated, and where learning from one another’s differences makes the whole better. AVF is comprised of many diverse people who are joining together to carry forth the mission of the AVF.
Sexism in Research and Publishing: A Trend on Its Way Out

Andrea Obi, MD
Chair, AVF Research Committee
Member, AVF Newsletter Committee
In the last decade increasing attention has been drawn to sex as a biologic variable (SABV). While human clinical trials have in recent times frequently involved men and women, sex was not routinely considered in preclinical study design and research often heavily relied on male animals. In 2016, the NIH began formally requiring that research design, analysis, and reporting in human and animal studies include SABV . The 5-year follow up of this initiative was published in 2020 in a paper published in the Journal of Women’s Health, “Sex as a Biological Variable: A 5-Year Progress Report and Call to Action.” (1)
Why is this important? Increasingly, it has been noted that the quality and completeness of medical research relies on taking sex into account. How can we expect that women will receive evidence-based disease prevention and treatment options if SABV is ignored? Addressing this issue is the overriding mission of the 2019-2023 Trans-NIH Strategic Plan for Women’s Health, which also aims to promote women in science careers to their full potential. In 2023, expect to see increasing accounting of SABV and inclusion of female animals in preclinical research.
References
1.ArnegardME, Whitten LA, Hunter C, Clayton JA. Sex as a biological variable: A 5-year progress report and call to action. J Womens Health (Larchmt) (2020) 29: 858-864.
2,800-Mile Step

Sebastian Cifuentes, MD
Member, AVF DEI Committee
Member, AVF International Committee
Mayo Clinic, Rochester
“A wise man ought always to follow the paths beaten by great men, and to imitate those who have been supreme, so that if his ability does not equal theirs, at least it will savor of it.”
-Niccolo Machiavelli
The only constant in life is change. As years passed during medical training in Colombia, I realized that medicine, particularly vascular surgery, was more than a profession or a job. Instead, I conceived it to be a lifestyle and my utter purpose. Naturally, a definite purpose requires a thoughtful plan. The main questions I would ask myself were how and where I would reach my full potential to better serve my future patients, the specialty, and humanity. After extensive meditation, I decided to pursue my career in the United States.
Transitions are fueled by the passion for your goal and demand sacrifice and responsibility. Leaving behind my country and family meant taking a challenging 2,800-mile step out of my comfort zone. This added a bittersweet taste to the process; however, changes always bring opportunity. It has been more than 6 months since I started a research position in the US, and the shift has undoubtedly been propitious.

Through this new chapter, I am grateful for the memories, friends, experiences, and achievements that life has granted me. The work ethic, quality of clinical care, scientific rigor, and kindness of the working team has greatly exceeded my expectations and has made the foremost scenario to begin a career in the United States. In March 2020, just before the COVID-19 outbreak, I had the opportunity to attend the AVF Annual Meeting as a medical student for the first time. Since then, I have found a welcoming academic community in the American Venous Forum. The AVF has provided my peers and me an opportunity to solidify our passion for vascular surgery, build strong relationships with contemporaries and seniors, and actively participate in its committees and yearly congress.
For those of my dearest early-career peers, this endeavor is just starting, and the pathway ahead is long and exciting. I do not doubt that relentless effort and discipline will put us in the right place at the right time to bring wellness and hope to our future patients. Finally, Dr. William Mayo said, “No one is big enough to be independent of others.” I owe my present to the many who have enlightened the pathway, taught, and guided me through the most significant decisions. I want to take advantage of these short lines to thank DrJorge H. Ulloa and Dr Todd E. Rasmussen–innovators, leaders, and mentors whose steps have left positive marks on the lives of many.
Rethinking Thrombolytics and Stand-alone Anticoagulation in the Age of Advanced Mechanical Thrombectomy for the Treatment of Deep Vein Thrombosis

Venkat Tummala, MD
Vascular Interventional Radiologist
VP Medical Affairs, Inari Medical
Field experience and newly published data often precede official guideline modifications, with physicians contributing to a groundswell of change as they experience success with and adopt new technologies. Such is the case with mechanical thrombectomy for deep vein thrombosis (DVT) treatment, where a growing body of evidence supports the expanded use of newer therapies.
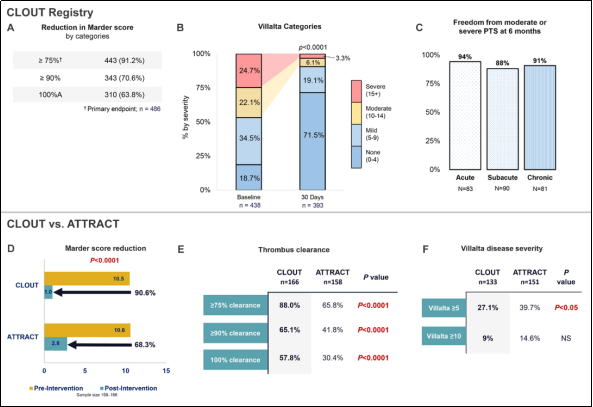
The ClotTriever® Thrombectomy System (Figure 1), a mechanical thrombectomy system designed to rapidly remove thrombus in a single session without the need for thrombolytics, has been used to treat more than 35,000 patients and is by far the most studied device to date with approximately 700 patients across 9 studies. (1-14) Results from the CLOUT registry, a 500-patient, prospective, all-comer study across 43 clinical sites, showed more than 90% complete or near-complete (>75%) thrombus removal (Figure 2A); 99% of cases were completed in a single session, with 0.0% incidence of major bleeding, valve or vessel damage, or acute kidney injury(11,12). Additionally, more than 90% of patients were free from moderate to severe post-thrombotic syndrome (PTS) symptoms at 30 days (11) and at 6 months (Figure 2B,C). (8) ClotTriever® has been shown to have none of the associated risks of bleeding from thrombolytics, excessive blood loss of continuous aspiration thrombectomy devices, or long-term procedure-related hospital and ICU stays.
To contextualize contemporary mechanical thrombectomy with historical treatment outcomes, a propensity-score matched analysis comparing results of CLOUT and the interventional arm of ATTRACT found that among 166 matched pairs, ClotTriever® produced superior thrombus extraction and lower Villalta scores at 30 days (Figure 2D-F). (13)
New tools to improve peripheral thrombus treatment continue to be developed. One such device is the Protrieve™ sheath (Figure 1), compatible with Inari platforms, which features a wall-apposing funnel designed to trap emboli during complex thrombectomy procedures involving the IVC. Another exciting new device that is now available is the InThrill™ Thrombectomy System (Figure 1), designed to remove acute to chronic thrombi and emboli in small 4-10mm vessels. The 8F system consists of a sheath with a recapturable, distal-braided funnel and a side port for aspiration, and a thrombectomy catheter with a self-expanding nitinol coring element.
Recently, success using InThrill™ as the front-line treatment to remove thrombus in the upper and lower extremities without significant blood loss or use of thrombolytics has been demonstrated.15 In a patient with thoracic outlet syndrome who presented with acute onset of left arm swelling and tightness, large pieces of highly organized thrombus in the left axillary and subclavian veins were removed using InThrill™. In another patient with complete occlusion of the left popliteal, femoral, and common femoral veins, InThrill™ was utilized to treat the below-the-knee and popliteal thrombus, which enabled left iliofemoral vessel access with ClotTriever®, and restored flow.
Conclusion
The new year is often a time to reflect on the past and take action to try new approaches. For DVT treatment, this means considering the breadth of data on innovative technologies with the potential to go beyond conservative therapies, leave high-risk thrombolytic treatments behind, and improve patient outcomes. New technologies in the Inari Medical toolkit should be part of this consideration, as they now make it possible to treat venous thrombosis throughout the peripheral vasculature.
Figure 2. A, data from the CLOUT registry show effective thrombus extraction as evidenced by reduced Marder Scores assessed by an independent core laboratory. (12) B,significant reduction in Villalta scores were seen at 30 days in the fully-enrolled, 500-patient CLOUT registry. (11) C, results at 6 months in the CLOUT registry 250-patient interim data set. (8)D-F, significant differences were seen in thrombus extraction and 30-day Villalta scores in a propensity-matched comparison of the CLOUT and ATTRACT interventional arm studies. (13)
References
- Benarroch-Gampel J, Pujari A, Aizpuru M, Rajani RR, Jordan WD, Crawford R. Technical success and short-term outcomes after treatment of lower extremity deep vein thrombosis with the ClotTriever system: A preliminary sxperience. J Vasc Surg Venous Lymphat Disord 2020; 8: 174–181. https://doi.org/10.1016/j.jvsv.2019.10.024.
- Zia S, Juneja A, Chadnick Z, Tan R, Neriah D, Singh K, Schor J, Deitch J. Provisional review and comparison of ClotTriever mechanical thrombectomy versus catheter directed and other mechanical thrombolysis and thrombectomy modalities for lower extremity deep venous thrombosis. J Vasc Surg 2020; 72: e243–e244. https://doi.org/10.1016/j.jvs.2020.04.403.
- Irshad,A, Shah P, Jain AK, Gifford E, Ayach M, Gallagher J, Divinagracia T. Promising novel technique for percutaneous extraction of chronic lower extremity deep venous thrombosis: Clinical cxperience with the ClotTriever system. J Vasc Surg 2020; 72: e60–e61. https://doi.org/10.1016/j.jvs.2020.04.110.
- Raskin A, Verma A, Brennan TD. Single-session thrombolysis-free treatment of deep vein thrombosis with a novel mechanical thrombectomy device. JACC Case Rep 2021; 3: https://doi.org/10.1016/j.jaccas.2020.12.049.
- Shah NG, Wible BC, Paulisin JA, Zaki M, Lamparello P, Sista A, Sadek M, Jacobowitz GR, Maldonado TS. Management of inferior vena cava thrombosis with the FlowTriever and ClotTriever systems. J Vasc Surg Venous Lymphat Disord 2021; 9: 615–620. https://doi.org/10.1016/j.jvsv.2020.09.008.
- Wadhwa V, Malhotra A, KesselmanA. Abstract no. 128. Rapid single-session mechanical thrombectomy of lower extremity deep venous thrombosis using the ClotTriever system: A single-institution experience. J Vasc Interv Radiol 2021; 32: S57. https://doi.org/10.1016/j.jvir.2021.03.134.
- Jolly MA, Lockhart MM, Shah D, Huff CM, Valenti EA, Phillips JA, Bittar S, Botti CF, Kolluri R, SilverMJ. Outcomes from a tertiary care center using a catheter thrombectomy system for managing acute iliofemoral deep vein thrombosis. J Vasc Surg Venous Lymphat Disord 2022; 10: 1044–1050. https://doi.org/10.1016/j.jvsv.2022.04.010.
- Dexter DJ, Kado H, Schor J, et al. Interim outcomes of mechanical thrombectomy for deep vein thrombosis from the all-comer CLOUT registry. J Vasc Surg Venous Lymphat Disord 2022; 10: 832–840. https://doi.org/10.1016/j.jvsv.2022.02.013.
- Weissler EH, Cox MW, Commander SJ, Williams ZF. Restoring venous patency with the ClotTriever following deep vein thrombosis. Ann Vasc Surg 2022. https://doi.org/10.1016/j.avsg.2022.07.031.
- Maldonado TS, Dexter DJ, Kado H, et al. Outcomes from the ClotTriever outcomes registry show symptom duration may underestimate deep vein thrombus chronicity. J Vasc Surg Venous Lymphat Disord. 2022;10:1251-1259. doi: 10.1016/j.jvsv.2022.04.015
- Dexter D. In-hospital and 30-day outcomes from the fully-enrolled multicenter prospective CLOUT registry. Presented at: The VEINS; October 31, 2022; Las Vegas, Nevada
- Dexter DDJ, Kado H, Shaikh ., et al. Safety and effectiveness of mechanical thrombectomy from the fully enrolled multicenter, prospective CLOUT registry. Journal of the Society for Cardiovascular Angiography and Interventions. In press.
- Abramowitz S. Propensity-score matched analysis of early clinical outcomes from the CLOUT and ATTRACT studies. Presented at: The VEINS; October 31, 2022; Las Vegas, Nevada
- Abramowitz S, Kado H, Schor J, et al. Six-month deep vein thrombosis outcomes by chronicity: Analysis of the real-world CLOUT registry. Journal of Vascular and Interventional Radiology. In press.
- Kumar V, Khanna P. First reports on the novel InThrill thrombectomy system. Endovascular Today 2022.
Thromboprophylaxis: An Often-forgotten Part of Endovenous Intervention

Benedict R.H. Turner
Section of Vascular Surgery, Charing Cross Hospital
Imperial College London, London, UK

Matthew Machin
Section of Vascular Surgery, Charing Cross Hospital
Imperial College London, London, UK

Professor Alun H. Davies
Section of Vascular Surgery, Charing Cross Hospital
Imperial College London, London, UK
Endovenous intervention for varicose veins is an ambulant procedure and is often thought to be associated with a low risk of venous thromboembolism (VTE) complications. However, the rate of deep venous thrombosis (DVT) is significantly higher compared to other day-case procedures of equivalent complexity and duration. The phenomenon may be due to perforator communications of deep and superficial lower limb veins that predispose patients to developing DVT or to endovenous heat-induced thrombosis (EHIT), which may result in associated morbidity through development of the post-thrombotic syndrome (PTS) and even mortality through embolization to the pulmonary vasculature. Deaths from pulmonary emboli (PE) after varicose vein procedures have been reported. As medical professionals, we can agree these are completely preventable deaths.
Depending on the series considered, the rate of DVT is seen to vary considerably. Our recent systematic review and meta-analysis considered the rate of DVT, PE, and major bleeding reported in published studies with the presence of pharmacological and mechanical thromboprophylaxis versus mechanical thromboprophylaxis alone. (1) We pooled data from 221 published articles; considering only the data from the 47 randomized controlled trials, the DVT rate with additional pharmacological thromboprophylaxis is more than 4 times lower (0.52%) (1095 patients, 2 events) than with mechanical thromboprophylaxis alone (2.26%) (6951 patients, 69 events). Interestingly, subgroup analysis demonstrated no differences in the DVT rate between the treated vein (great/ short/ anterior accessory saphenous) nor in the endovenous treatment modality utilized (cyanoacrylate glue/ endovenous laser/ foam sclerotherapy/ mechanochemical/ radiofrequency). Further, there were no differences between a single peri-operative dose of antithrombotic medication versus an extended course (range 2-13 days) post-operatively. Importantly, data were pooled from trial arms and there were no randomized trials that compared head-to-head pharmacological and mechanical thromboprophylaxis versus mechanical thromboprophylaxis alone.
The review did not address the actual role of compression therapy after endovenous interventions for varicose veins. UK national guidelines, as well as some manufacturers, recommend graduated compression stockings (GCS) for one week after endovenous ablation. The role of compression here is theoretically multiple: as an adjunct for venous closure; to reduce post-procedural swelling and pain; and as a form of mechanical thromboprophylaxis. (2) However, a systematic review of the efficacy of GCS in addition to pharmacological thromboprophylaxis undertaken by the authors (and currently under peer review) has demonstrated no additional benefit of GCS, in line with the results of the GAPS trial. (3, 4) While the immediate application of compression bandaging for procedural efficacy and post-procedural pain is warranted, can we really recommend the prolonged prescription of GCS?
The above information has led to the establishment of an NIHR-funded trial to look at the benefits of pharmacological thromboprophlaxis in patients undergoing endovenous treatment for varicose veins. Pending the results of this study, we would recommend formal assessment of patients with a risk assessment tool and VTE prophylaxis decisions should be based on this. Patients need to be made aware of the risk of VTE.
References
- Turner BRH, Machin M, Jasionowska J, et al. Systematic review and meta-analysis of the additional benefit of pharmacological thromboprophylaxis for endovenous varicose vein interventions. Ann Surg2022; Sep 15. Epub ahead of print. PMID: 36205129
- Bootun R, Belramman A, Bolton-Saghdaoui L, et al. Randomized controlled trial of compression after endovenous thermal ablation of varicose veins (COMETA rrial). Ann Surg. 2021;273:232-239.
- Turner BRH, Machin M, Jasionowska J, et al. Systematic review and meta-analysis of graduated compression stockings in addition to pharmacological thromboprophylaxis for surgical inpatients. Unpublished,
- Shalhoub J, Lawton R, Hudson J, et al. Graduated compression stockings as adjuvant to pharmaco-thromboprophylaxis in elective surgical patients (GAPS study): randomised controlled trial. BMJ. 2020; 369:m1309.
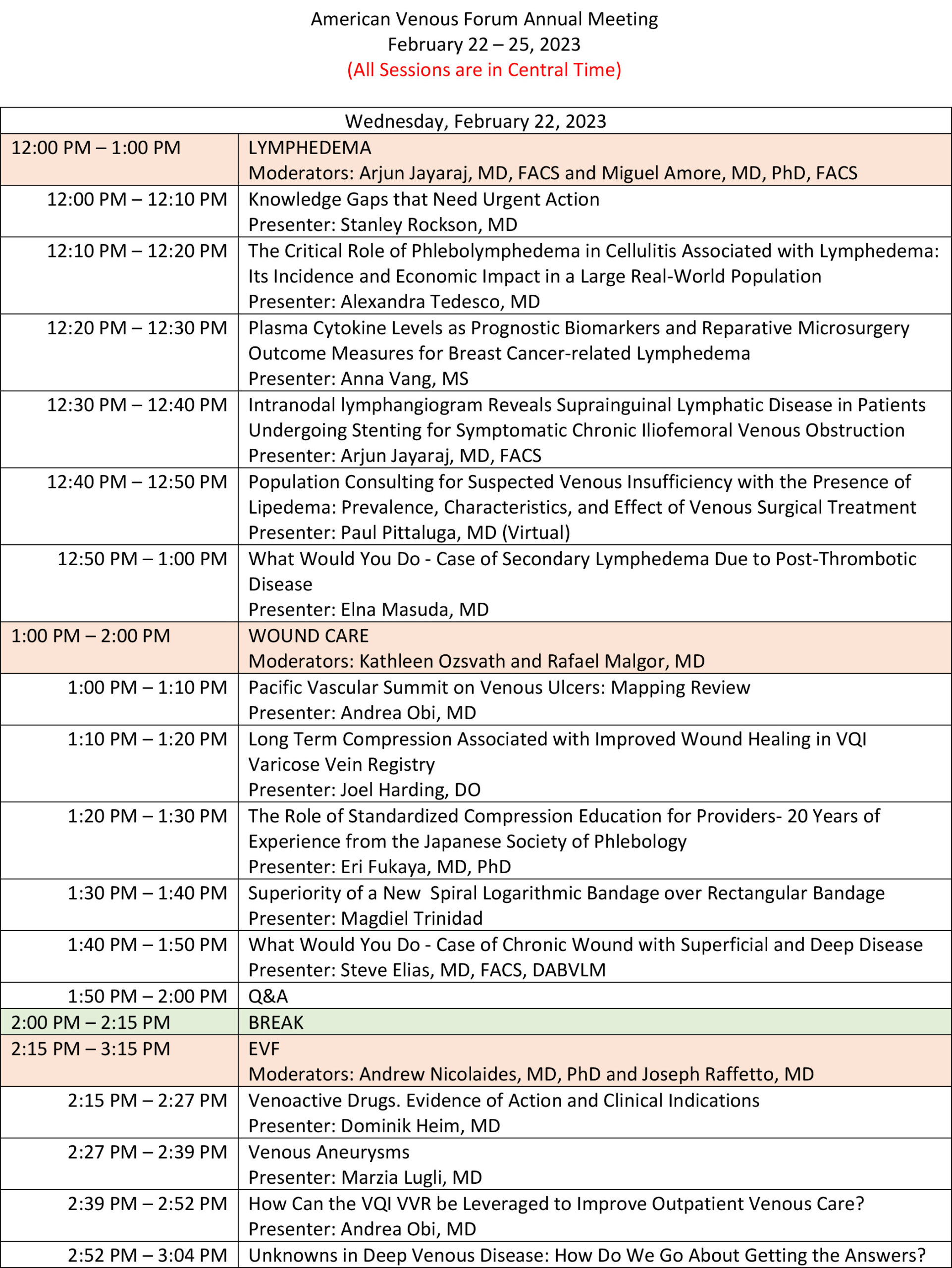
VENOUS2023 Full Agenda
Kick Off Your Boots at the VENOUS2023 Gala!
Join us at VENOUS2023!

The AVF partnered with Venous Edge to promote the AVF’s upcoming annual meeting, VENOUS2023. Steve Elias, MD has moderated a short video featuring Mikel Sadek, VENOUS2023 Program Chair; Bill Marston, President of the American Venous Forum; Julianne Stoughton, Aesthetic Session Chair; and Angela Kokkosis, VENOUS2024 Program Chair. Learn more about VENOUS2023 and why you don’t want to miss this event!
Click here to watch the video. Flip to page 12 of Vol. 2, Issue 6.
Poster Session at VENOUS2023

Nasim Hedayati, MD, MAS, MS
Member, AVF Annual Meeting Committee
Member, AVF Early Career Committee
As we prepare for the VENOUS2023 meeting in San Antonio, Texas, we wanted to introduce our members and colleagues to one of the exciting programs at the Annual Meeting–the Poster Session. As always, this session is an integral part of our meeting. Many of us remember our very first exposure at a national meeting as a medical student or as a trainee who was presenting a poster! We stood nervously by our poster and answered the questions of people we admired and the surgical giants we had only heard of. We want to recreate that magic in person for all those great works that have been accepted to present this year.
This year, the poster session has high quality abstracts from around the world that were selected from an amazing group of submissions. This blinded process was highly competitive. The in-person poster session presenters will have a chance to present their work in front of judges and conference attendees and will be eligible for poster awards. Each presenter will have a 3-minute presentation followed by 2 minutes for questions and answers. These posters as well as the virtual posters will be available on our meeting portal. Only the in-person posters will be eligible for the awards.
The posters will be available for viewing in the foyer throughout the meeting. The poster session will take place on February 24th from 3:15 pm to 4:45 pm CT in the foyer of La Cantera Resort. We hope to see you there.
Take a look at the amazing abstracts that will be presented this year:
| Poster # | Presenter | Submission Title | Submission Topic |
| 1 | Nadiv Shapira, MD | Lymph Sparing Liposuction in Treating Lipedema: How and Why | Lymphedema |
| 2 | Miguel Amore, AA | Near-Infrared Fluorescence Imaging in Lymphatic/Chylous Diseases | Lymphedema |
| 3 | Matthew Melin, NF | Congestive Lower Extremity Failure; an educational model for improved understanding of Phlebolymphedema | Miscellaneous |
| 4 | Perry Kerner, PU | Topical Oxygen Therapy for Chronic Venous Stasis Ulcers in Patients Who Failed Multiple Prior Therapies | Wound Care |
| 5 | Amr Mahmoud, FU | Effect of sub-ulcer venous plexus injection by foam sclerotherapy to heal active venous ulcer | Wound Care |
| 6 | Aoi Ogawa, AH | Imaging differences between non-thrombotic iliac vein lesion and post-thrombotic syndrome | Chronic Vein Obstruction/Compression |
| 7 | Valentyna Kostiuk, NY | A Novel Dedicated Endovascular Grasper Can Decrease Procedural Time and Facilitate Challenging Inferior Vena Cava Filter Retrieval | Venous Thromboembolism/IVC Filters |
| 8 | Jason Storch, TS | Patients with the Chief Complaint of Pigmentation Changes Present with More Severe Disease and Have Poorer Outcomes Following Iliac Vein Stent Placement | Chronic Vein Obstruction/Compression |
| 10 | Halbert Bai, GS | Higher Preoperative Venous Clinical Severity Scores are Not Associated with More Major Reoperations | Chronic Vein Obstruction/Compression |
| 11 | David Dexter, NS | Management and outcomes of symptomatic IVC atresia in the endovascular era | Chronic Vein Obstruction/Compression |
| 12 | Lukasz Kruszyna, EP | The Clinical Outcomes of the Patients with Venous Thoracic Outlet Syndrome Treated with Surgical Decompression | Venous Thromboembolism/IVC Filters |
| 13 | Kevin Engledow, DT | Endophlebectomy with Venous Stenting: An Underutilized Hybrid Option for Occlusive Chronic Femoral Venous Thrombosis | Chronic Vein Obstruction/Compression |
| 14 | Jan Kesik, MP | Tumor in the common femoral vein found prior to EVLT. What is the best approach? | Chronic Vein Obstruction/Compression |
| 15 | O Jesse Mendes, MH | Hemodialysis Access Salvage in the Setting of Central Venous Outflow Obstruction | Chronic Vein Obstruction/Compression |
| 17 | Sebastian Cifuentes, FC | Inferior Vena Cava and Bilateral Common Iliac Endovascular Revascularization For Refractory Post-Thrombotic Syndrome | Chronic Vein Obstruction/Compression |
| 18 | Andres Figueroa, NS | Venous Return and Orthostatic Hypotension A Case Report | Chronic Vein Obstruction/Compression |
| 19 | Maria Santa Cruz, CY | Increased Lower Extremity Pain during Menstruation in Patients with Chronic Venous Insufficiency | Superficial Vein Disease |
| 20 | Wilhelm Dr. Sandmann, TG | Nutcracker and MAY-THURNER Syndromes: Decompression by extra venous tube grafting and significance of hypermobility related disorders. | Chronic Vein Obstruction/Compression |
| 21 | Johann Ragg, RG | Perivenous injection valvuloplasty in congenital venous valve lesions | Superficial Vein Disease |
| 22 | Ali Basil Ali, CH | Recurrent Recanalization After Endovenous Thermal Ablation for Recanalized Varicose Veins | Superficial Vein Disease |
| 23 | Kate Gates, MD | Prevalence of venous disease in population with high occupational risk | Superficial Vein Disease |
| 24 | Kathleen Gibson, MD | The Novel Primary Endpoints of the VenaSeal Spectrum Study: Peri-Procedural and Subsequent Treatment Satisfaction as Measured by the Venous Treatment Satisfaction Questionnaire, and Elimination of Truncal Reflux | Superficial Vein Disease |
| 25 | Mitsumi Yamashita, AJ | Evaluation of radiofrequency ablation system for branch varicosities | Diagnostic Testing and Imaging |
| 26 | Takaya Murayama, LJ | Sclerotherapy for pulsatile phlebitis due to micro arteriovenous fistulas | Superficial Vein Disease |
| 27 | Erasto Aldrett, SM | OBSERVED DIFFERENCES BETWEEN 980 nm AND 1470nm ENDOVENOUS LASER TREATMENT ON CEAP 4-5-6 PATIENTS | Superficial Vein Disease |
| 28 | Antonio Solano, RS | Varicosities as A Sign of Hidden Diseases | Superficial Vein Disease |
| 29 | Johann Ragg, EG | Prevention in Phlebology – Results of PREVENT2 | Superficial Vein Disease |
| 30 | Mehernosh Gardin, RI | VARICOSE VEINS TREATED WITH ENDOVENOUS LASER ABLATION –
A RETROSPECTIVEAND ON-GOING PROSPECTIVEOBSERVATIONAL STUDY |
Superficial Vein Disease |
| 31 | Megan Lombardi, OC | Spontaneous Resolution of Left Common Iliac Vein Compression After Acute DVT In a Teenager without Stenting | Chronic Vein Obstruction/Compression |
| 32 | Benedict Turner, UK | An updated systematic review and meta-analysis of the additional benefit of graduated compression stockings to pharmacologic thromboprophylaxis in the prevention of venous thromboembolism in surgical inpatients | Venous Thromboembolism/IVC Filters |
| 33 | Oscar Moreno Rocha, RM | First Human Study to Assess the Safety of Selectin Inhibitor Uproleselan (GMI-1271) in Patients with COVID-19 Severe Pneumonia | Venous Thromboembolism/IVC Filters |
| 34 | Drew Braet, TM | Outcomes Associated with Procedure Type After Superficial Venous Procedures | Superficial Vein Disease |
| 35 | Ali Basil Ali, DH | Endovenous Percutaneous Mechanical Thrombectomy of Inferior Vena Cava Occlusive Tumor Thrombus Using ClotTriever Device | Venous Thromboembolism/IVC Filters |
| 36 | Nicholas Anderson, SS | Risk of Major Bleeding with Pulmonary Embolism Therapy: A Systematic Review and Model-Based Meta-Analysis | Venous Thromboembolism/IVC Filters |
| 37 | Nicolas J Mouawad, MD MPH MBA | The Impact of Stenting After Mechanical Thrombectomy for Postthrombotic Syndrome-Associated Venous Leg Ulcers | Chronic Vein Obstruction/Compression |
| 38 | Allie Olmstead, CH | A Comparison of Dedicated vs Non-Dedicated Venous Stents Following Thrombus Clearance in Patients with Acute Iliocaval and Ileofemoral Deep Venous Thrombosis | Chronic Vein Obstruction/Compression |
| 39 | Hilary Hayssen, EM | The need for standardizing the use of the Caprini Risk Assessment Model to assign risk for venous thromboembolism | Venous Thromboembolism/IVC Filters |
| 40 | Chase Hoffman, EH | Seeing is Believing – But You Need to Look! | Venous Thromboembolism/IVC Filters |
| 41 | Guillermo Tafur, LU | Pulmonary Embolism Mortality Among Heart Failure Patients: Analysis of the National Inpatient Sample Database | Venous Thromboembolism/IVC Filters |
| 43 | Chase Hoffman, UH | Unusual Cause and Presentation of Paradoxical Embolus After Elective Hip Arthroplasty | Venous Thromboembolism/IVC Filters |
| 44 | Alexandra Mansour, SM | Risk Determination in Postpartum Obstetric Patients for Venous Thromboembolism | Venous Thromboembolism/IVC Filters |
| 45 | Roger Kayaleh, DP | Medicare Services Utilization Trends in the Treatment of Superficial Venous Disease. | Superficial Vein Disease |
| 46 | Joann Lohr, SVA | Positive Impact of a Quality Assurance Program | Vascular Medicine |
| 47 | Jason Storch, TS | Extreme Outliers in BMI Reveal Differences in Outcomes Following Iliac Vein Stenting | Chronic Vein Obstruction/Compression |
| 48 | Halbert Bai, ES | Preoperative VCSS Pain, Varicose Veins, and Pigmentation are Significant Predictors of Major Reoperation | Chronic Vein Obstruction/Compression |
| 49 | Jason Storch, IS | Iliac Vein Stenting for Proximal Venous Outflow Obstruction in Cancer Patients is a Safe and Durable Palliative Therapy | Chronic Vein Obstruction/Compression |

Photos from the Poster Session at VENOUS2022 in Orlando, FL.
DEI Session Invitation

Sheila Blumberg, MD, MS, RPVI
Member, AVF DEI Committee
Come one, come all, to the “One World, Many Voices” DEI session at the 35th Annual American Venous Forum meeting. The AVF Diversity, Equity, and Inclusion Ad Hoc committee kindly invites you to join us for these finely curated and enlightening topics spanning the depth and breadth of DEI issues in the diagnosis and treatment of venous disease from our esteemed colleagues and experts. Please join us for a lively discussion and become part of the solution! See you in San Antonio on Thursday, February 23 from 10:15 – 11:45 am CT.
One World, Many Voices DEI Session Moderators
Misaki Kiguchi, MD
Kathleen Ozsvath, MD
Sheila Blumberg, MD, MS
- Session Introduction – DEI Foundation, Vision & Mission presented by Sebastian Cifuentes, MD
- How Do We Encourage Insurance Companies to STOP Excluding Patients from Payment? Example Varicocele vs Pelvic Venous Disease presented by Kathleen Ozsvath, MD
- Importance of Sensitivity to Patients’ Individual Backgrounds in Venous Care presented by Faisal Aziz, MD
- What Can We Learn from Each Other on an International Level? presented by Rebeca Reachi, MD
- An Analysis of Endovenous Ablation Procedures by Provider Type, Including Advanced Practice Providers: A Study Using the Medicare Fee-for-Service Database presented by Mikel Sadek, MD
- Venous Insufficiency in Children and Adolescents: Progression Over 4 Years presented by Johann Ragg, MD
- Race/Ethnicity and Outcomes of Venous Ablation Procedures presented by Nikita Singh, MD
- The Population Burden of Chronic Venous Disease in the United Kingdom presented by Safa Salim, PhD, MBBS
- Panel featuring Karem Harth, MD, Anil Hingorani, MD, Elna Masuda, MD, and Ruth Bush, MD, JD, MPH
A Welcome Reception You Don’t Want to Miss!
The Welcome Reception at VENOUS2023 promises to be enjoyable and memorable. The reception will take place Thursday, February 23, 2023, at our meeting venue, La Cantera Resort in San Antonio, Texas. Enjoy libations, meet new friends, and reconnect with old friends at this year’s Welcome Reception! All attendees are invited to attend and enjoy some time together as we all strive to advance the mission of the AVF by caring for patients with venous disease.
This year, we are adding two special events within the Welcome Reception: the AVF International Reception and the AVF New Member Reception!
International Reception
Antonio Solano, MD
Member, AVF Digital Media Committee
For the first time, the AVF will host a special reception for our international attendees who travelled a great distance to join us at VENOUS2023! The International Reception aspires to be delightful and memorable. We anticipate that attendees from all around the world will be found to socialize, network, and enjoy splendid refreshments throughout the evening during this event. It is an opportunity to share with other peers our culture, beliefs, and ideals that make us unique.
Throughout this meeting, the AVF hopes to strengthen the academic, cultural, and camaraderie bonds among international peers. Diversity enriches our society and science, and the AVF strives to nurture friendship and knowledge to enhance the care of patients with venous disease.
Photo from the International Reception at VENOUS2022.
New Member Reception
The AVF is thrilled to welcome all new members to the VENOUS2023! If you are new to the AVF, please keep an eye out for our special New Member area. Be sure to stop by to meet fellow new members, as well as some of the AVF’s leaders who are eager to welcome you to the society.
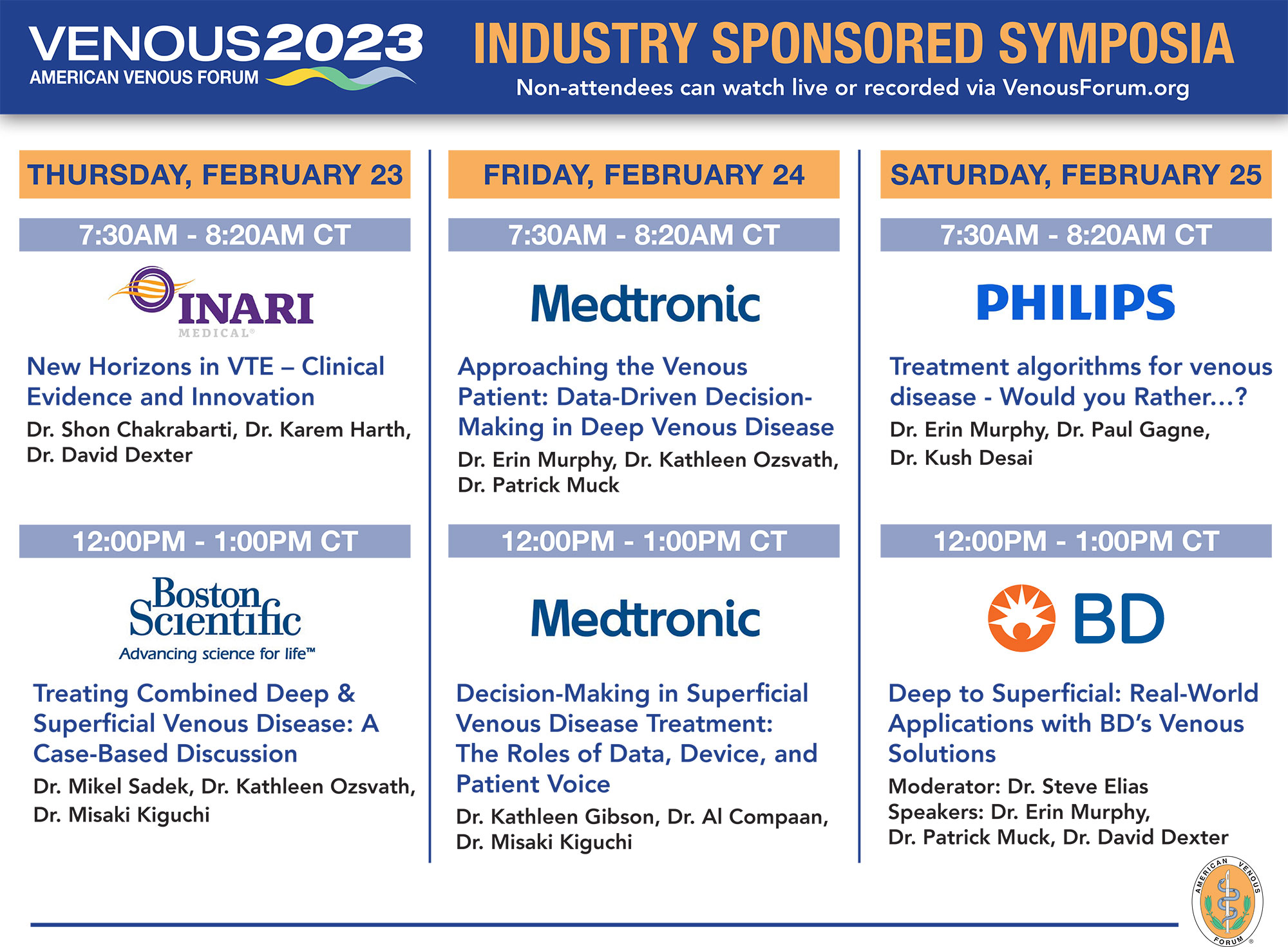
Medtronic Symposium Invitation

Stephanie Brucato
Scientific Communications Program Manager at Medtronic Peripheral Vascular Health

Daniel J. Denmark, PhD, MS
Scientific Communications Program Specialist at Medtronic Peripheral Vascular Health
On Friday, February 24, Medtronic will sponsor a lunch symposium at VENOUS2023 focused on therapy for superficial vein disease (SVD). The title of that symposium is “Decision-Making in Superficial Venous Disease Treatment: The Roles of Data, Device, and Patient Voice.” The moderator will be Dr Kathleen Gibson. She will be joined by a patient and also by Dr Misaki Kiguchi.
This symposium will bring attention to the voice of patients. Despite the many tools for collecting patient feedback, there is no questionnaire that asks the patient how they are doing around the time of a superficial vein procedure. The VenaSeal™ Spectrum Program uniquely introduces the Venous Treatment Satisfaction Questionnaire (VenousTSQ). This new tool assesses patient treatment satisfaction. During the program Dr. Gibson will interview her patient to determine the things that were important to him when selecting a particular superficial vein treatment modality. The patient will discuss his history with SVD, the research he conducted in making his decision, advice he would give to other patients, and his impression of the treatment he received.
Dr Kiguchi will then give an overview of the VenaSeal™ Spectrum Program, which is made up of 3 separate studies. The VenaSeal Spectrum Endothermal Ablation (ETA) Study is a randomized controlled trial (RCT) that will evaluate participants receiving VenaSeal versus those receiving ETA. The VenaSeal Spectrum Surgical Stripping Study, another RCT, will look at participants receiving VenaSeal versus those receiving surgical stripping. The VenaSeal Spectrum Venous Leg Ulcer Study is a single-arm study following participants with advanced SVD, or venous leg ulcers, after VenaSeal treatment. Aside from the unique VenousTSQ assessment, Dr Kiguchi will also describe how the elimination of truncal reflux will be used as a novel primary endpoint in the first 2 studies, while conventional measures like closure rate and return-to-work are reported as secondary endpoints. Dr Kiguchi will conclude her presentation with a patient case.
To close the symposium, Dr.Gibson will present the very first data from the VenaSeal Spectrum Program. This will include the baseline demographics from the first 100 US-English speaking participants that responded to the VenousTSQ. Those responses will be used to validate the VenousTSQ through psychometric analysis. Dr Gibson will describe the baseline demographics, what progress has been made in psychometric analysis so far, and the implications of what the VenousTSQ will mean for SVD treatment and research. Dr Gibson will also present a patient case.
Medtronic will also sponsor a breakfast symposium on the same day that will focus on deep vein disease therapies. Data on the treatment of iliofemoral venous outflow obstruction with dedicated venous stents through 3 years is now available. The panel will discuss key differences in the venous stent IDE trials with specific attention given to the recently released 36-month data from the ABRE Study. Included in the discussion is the physician’s approach to treating the venous patient in concert with the available data.
Come enjoy breakfast and lunch on February 24 and watch these exciting symposia!
Introduction to the German Society of Phlebology

Erika Mendoza, MD
President, European Venous Forum
The German Society for Phlebology was founded on 24 March 1957 in the Hotel Frankfurter Hof in Frankfurt am Main as the “Working Group for Venous Diseases (Phlebology).” At the same time, the first conference of the newly founded working group, whose origins go back to the Verein der Spezialärzte für Beinleiden (Society of physicians specialized on leg illnesses 1909-1934), took place here. Initially, the name “Society” was deliberately avoided to prevent a further division of the field of cardiovascular diseases. Further founding ideas were to unite science and practical aspects, as well as trainings and to integrate “Phlebology” as one specialization in the large field of vascular diseases. The society has developed scientific publications in the field of phlebology since 1961, after the foundation of the UIP (Union international de Phlébologie) in 1959. The first president of the UIP was Erich Krieg, from Germany, and he served as host of the 2ndInternational UIP Meeting 1965 in Wiesbaden. Since 1990 the name of the Society has been Deutsche Gesellschaft für Phlebologie (German Society of Phlebology), with Phlebologie as our scientific journal.
While about 200 people attended the second conference in October 1957, the DGP has since grown to more than 1,900 members. In 2022 at our latest conference in Hanover, the fusion between the DGP and the DGL (German Society of Lymphology) was established. The new society will be composed of 2800 members and is one of the largest lympho-phlebological scientific organizations worldwide.
The most important topics the society addresses are scientific and educational. Since its foundation, 64 annual meetings have been organized all over Germany. In 2009 the meeting was in conjunction with the UIP and the French Society of Phlebology in Monaco. The society is responsible for the guidelines of venous treatments, participating in thrombosis treatment and prophylaxis guidelines as well as lymphology guidelines in the past. The society is involved in the postgraduate training of phIebologists. In Germany, phlebology is a specialization, available to general practitioners, internists, surgeons and dermatologists. It requires 18 months of postgraduate training in specialized centers, developing and adapting to political changes in the German system, where the phlebologic activities are more and more moving from hospitals to offices. One of the latest achievements was a Certificate of Continuous Training in the Field of Phlebology, taking into account the fact that phlebology is developing very quickly and to ensure that doctors who treat patients and bill health insurance companies have a permanently high standard.
The German Society of Phlebology will be the host of the upcoming meeting of EVF June 22-24, 2023.

René Haegerling (President of German Society of Lymphology (DGL) and new member of the Board of DGPL), Anya Miller (Former President of the DGL and member of the scientific Board of DGPL), Markus Stücker (President of the DGPL) and Erika Mendoza (General Secretary of DGPL) (from left to right) cutting the Wedding Cake at the German Society Meeting in September 2022 in Hannover
Welcome New AVF Members!
November/December
| Name | Country |
| Katherine Hekman | United States |
| Katherine Teter | United States |
| Phung Le | United States |
| Luis Suarez | United States |
| Shahriar Alizadegan | United States |
| Lalit Nirwan | India |
| Ashna Raiker | United States |
| Ricardo Rodriguez | Mexico |
| Sergio Flores Cantu | Mexico |
| Sreekumar Madassery | United States |
| Daniel Goldberg | United States |
| Ana Botero | Colombia |
| Jake Hemingway | United States |
| Lukasz Szczygiel | Poland |
| Lourdes Reina-Gutierrez | Spain |
| Alexandra Fairchild | United States |
| Lukasz Kruszyna | Poland |
| Pablo Castro | Argentina |
| Jorge Garcia-Davila | Mexico |
| Christina Guarin | United States |
| Jan Kesik | Poland |
| Jacob Wood | United States |
| Martin Cargnan | United States |
| Ashley King | United States |
| Ana Ferrufino | Mexico |
| Jennifer Thomas | United States |
| Lorena De Marco Garcia | United States |
| Nishant Agrawal | United States |
| Elias Fakhoury | United States |
| Nicole Rich | United States |
| Mary Knott | United States |
AVF Health Policy Committee at Work for You
AVF Health Policy Committee
Dear Colleagues,
With all the attention appropriately focused on Medicare (labor update, conversion factor, budget neutrality, etc.), it would be easy to lose sight of commercial insurance varicose vein coverage policies. However, rest assured the AVF Health Policy Committee in collaboration with the SVS and AVLS continues to support our members, as you address policies and denials that are at times capricious and others systematically restrictive. Among the most egregious policy is the long standing BCBS North Carolina Policy restricting venous procedures to one vein, per leg per life. We continue to push for a change to this policy at the regional and national level. See our latest letter to BCBS. We have and will continue to be responsive to communications from our members, who receive unjust denials or are faced with perverse policies. If this has happened to you, please post in the AVF exchange or email [email protected].
During the last year, the Health Policy Committee adopted a more proactive approach. Leveraging our powerful new tool, Policy Navigator, we have up-to-date venous policy documents for all commercial and private payors in the US. Not only can we quickly review current policies, we can see proposed changes and respond in time to affect policy. The Venous Policy Navigator is available for use in your office and can greatly reduce the work required to stay on top of the rules of the road in your region. Learn more about Policy Navigator here.
The AVF Health Policy committee is committed to supporting venous practitioners in your efforts to bring high quality care to your patients and to ensure that reimbursements systems support continued access to care. Let us know how we can help you.
Sincerely,
The AVF Health Policy Committee